Surrey care home fined £25k after resident head injury death

A care provider has been ordered to pay £24,981 after it failed to protect a person living in one of its services from significant risk of avoidable harm.
This comes via the Care Quality Commission (CQC), regulator of most health and care services in England, which revealed that the provider found itself in court last week (15 May).
Claremont Care Services, the provider in question, was also found to have failed to inform and apologise to resident John Bowles’ family following his death.
The company pleaded guilty to failing to provide safe care and treatment to Bowles, resulting in him being exposed to significant risk of harm which ultimately led to his death.
Brighton Magistrates’ Court fined the provider £24,800. It was also ordered to pay a £181 victim surcharge. Costs to the Care Quality Commission (CQC) which brought the prosecution will be determined at a later date.
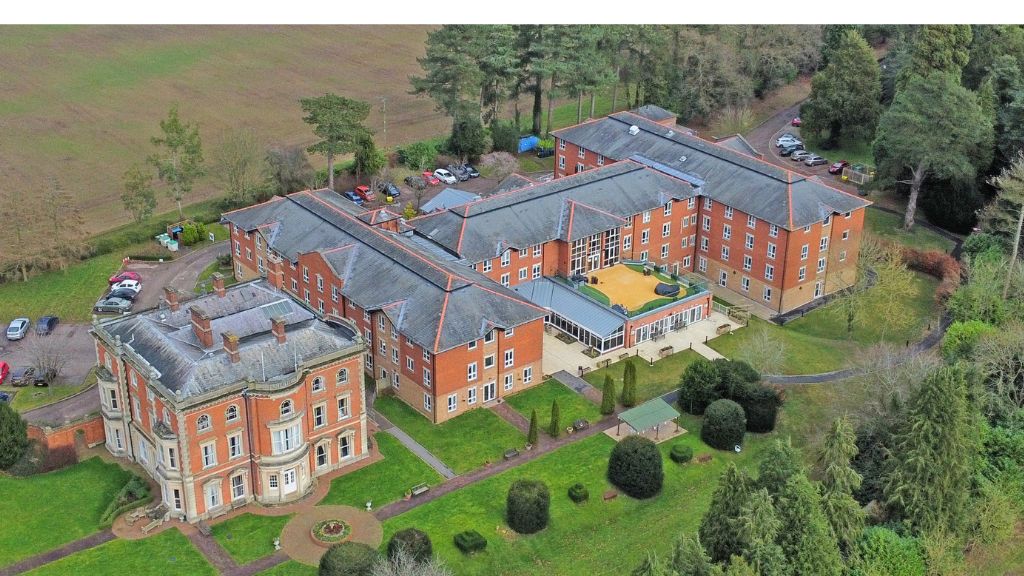
At the time of the incident, Claremont operated two care homes, including Offington Park Care Home in Worthing, which provided accommodation for up to 24 people.
On 25 December 2019, 75-year-old Bowles was admitted to the service after being discharged from hospital. When being discharged, the hospital told the home that Bowles was at risk of falls.
The provider was also made aware that Mr Bowles was taking medications which decreased blood clotting (anticoagulants). The National Institute for Health and Care (NICE) Guidelines advises that people on anticoagulants face greater risk from head injuries and should be urgently referred to hospital if they are injured in this way.
Mr Bowles suffered an unwitnessed fall on the day of his admission, but no injury was recorded. Three days later he suffered another unwitnessed fall and developed a lump on his head. He was taken to hospital where a scan found no head injury. This was the only time medical treatment was sought for Bowles following a fall.
Up to 8 February 2020, Bowles fell a further seven times, three of which caused him a head injury, but staff sought no medical treatment.
On the morning of 9 February 2020, he suffered another unwitnessed fall resulting in a head injury. Staff took physical observations but didn’t have any previous recordings to compare against. They offered to contact emergency services, but Bowles declined, and staff complied with his wishes, despite this going against NICE guidelines.
Later that evening, staff heard a loud bang from Bowles’ room. He said he banged the back of his head on the wall. Staff didn’t see an injury and didn’t seek medical treatment. A few hours later that night, staff found him walking in the corridor. He requested a specialist and staff offered to call emergency services but again he declined.
The next morning, staff found Bowles unresponsive in bed and called 999. He was pronounced dead at hospital and was later determined to have died from a traumatic head injury.
It was found that the service’s falls and head injury guidance didn’t advise staff to seek emergency care for people on blood thinning medication if they suffered a head injury. This is contrary to NICE guidelines. Bowles’ care plan was also incomplete and did not reflect the number of falls he had suffered. A falls risk assessment was not completed until he’d already fallen five times.
The provider also failed to inform and apologise to Bowles’ family soon enough after the incident and his death. In doing this, the provider has failed to fulfil their duty of candour.
Natalie Reed, CQC deputy director of operations in the south, said: “Our sympathies are with Mr Bowles’ family following his potentially preventable death.
“People receiving care and treatment have the right to expect that any risks to their safety will be effectively managed and families or loved ones will be informed in an open and transparent manner as soon as possible.
“The failure of Claremont Care Services to manage Mr Bowles’ risks and ensure that they were following national guidance essential to his safety and wellbeing was unacceptable. Furthermore, the lack of openness and transparency shared by Claremont to his family just added distress.
“The majority of care providers do an excellent job. However, when a provider puts people in its care at risk of harm, we will take action to hold them to account and to protect people.
“I hope the outcome of this prosecution reminds care providers of their duty to assess and manage all risks to ensure people are kept safe and families and loved ones are kept informed.”